The Dictionary of Sydney was archived in 2021.
Epidemics
Citation
Persistent URL for this entry
To cite this entry in text
To cite this entry in a Wikipedia footnote citation
To cite this entry as a Wikipedia External link
Epidemics
Many epidemics have swept Sydney since white settlement. As a port city through which millions of travellers, visitors and immigrants have passed, it has always been susceptible. Until the middle of the twentieth century, such epidemics were seen as part of life, something that everyone might have to face at some stage.
This understanding did not change until around World War II. [media]A range of medical developments from the late 1920s, such as the appearance of sulphonamide (in the 1930s), penicillin treatments (in the 1940s), inoculations and vaccinations (such as the Salk vaccine for polio in the 1950s), on top of existing strict quarantine regulations, fostered the belief that medical science had at last got a range of diseases under control. After World War II, Sydneysiders grew up feeling secure in the belief that epidemics were a thing of the past.
Dealing with epidemic disease
Reactions have varied to the epidemics that have swept the city over more than 200 years. Yet social responses to epidemics show a number of constants: initial panics; confusion among the various authorities about how best to deal with the disease; searches for causes that often spilled over into searches for scapegoats; and policies that sacrificed individual rights and liberties with little apparent compunction. After it was over, there was always soul-searching and questions such as 'where did we go wrong?' and 'how could we have better dealt with it?'
What usually emerged was that, repeatedly, public health services were unable to deal with the sudden onslaught of a new epidemic. Often, medical science could not provide immediate answers as to cause and point of origin, and as a result, health authorities tended to respond to political pressures, rather than medical realities. Demagogues could determine public policies, and charlatans and quacks had a field day.
But, paradoxically, there were often long-term beneficial results from these epidemics: improved medical techniques for dealing with disease and a heightened public awareness of the situation of minority groups, often changing attitudes to those groups and their problems. Of course, there were also very real costs too including death, misery and social and economic dislocation.
Understanding epidemics
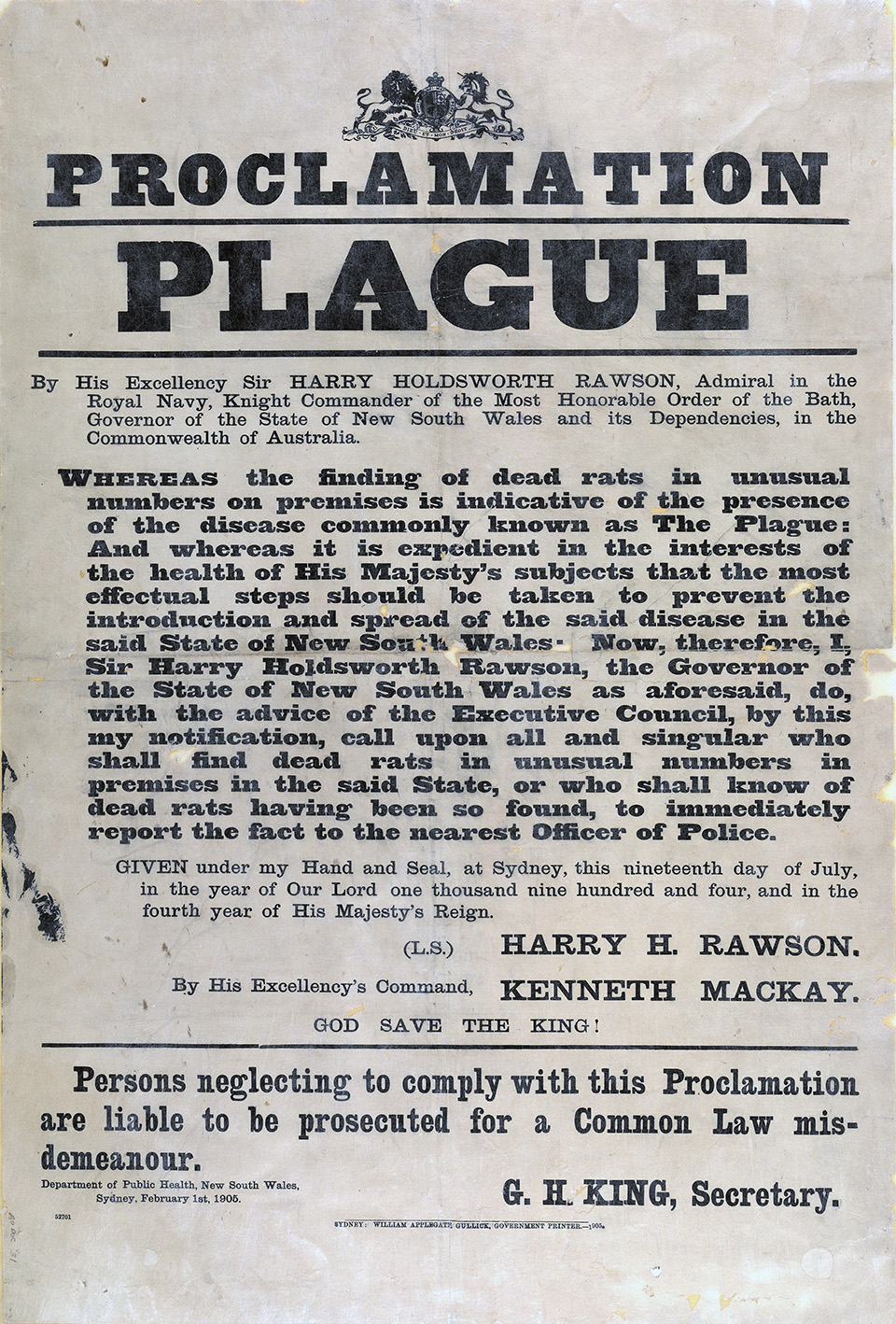
In its short two centuries of white history, Sydney has experienced many epidemics. Within the first few years, there was an epidemic of smallpox (or chickenpox), and this was followed by others, of which the measles epidemic in 1867, the scarlet fever epidemic of the 1870s, the smallpox epidemic of 1881–82, the Asiatic flu pandemic of 1890–91, the plague in 1900, and the Spanish influenza epidemic of 1918–19 were the worst. Later in the twentieth century came AIDS.
All of these have had a major impact on life in Sydney, some more than others. But they all have a tale to tell, and they show that an outbreak of disease may be perceived as an epidemic, even if it does not, in medical terms, constitute an epidemic. If a city sees something as a catastrophe, it may well become that catastrophe. While medical science defines an epidemic in terms of morbidity and mortality rates, these may not be the crucial factors in the public perception. Other factors clearly impinge. There is also the contrast with hangover infections from the nineteenth century, like polio, diphtheria and tuberculosis, which, while still causing fear and trepidation in the city well into the twentieth century, never caused the panic that other epidemics caused. These diseases, however devastating, were known quantities, so that the fear of the unknown was never as pressing.
[media]Although epidemics might have killed relatively few people, even if they incapacitated many thousands, the problem was exacerbated when they 'created an environment of bewilderment, panic and resentment.' [1] This in turn generated some of the extreme social responses that occurred. Very different public responses can be seen by comparing the 1881–82 smallpox epidemic (163 cases, with 41 fatalities) and the 1890–91 Asiatic flu pandemic (tens of thousands of cases, with 234 deaths). Yet it was smallpox that prompted widespread panic in Sydney, and highly exaggerated responses from both the public and the authorities. The Asiatic flu caused far greater dislocation to the city's economic and social life, and was undoubtedly accompanied by a considerable sense of helplessness and bewilderment, but it sparked relatively little of the panic and hysteria that were evident 10 years earlier, and would recur later with the appearance of the plague in Sydney in 1900.
With hindsight it is clear that the way the disease or epidemic is dealt with in its initial stages is crucial. Indecision, confusion, conflicting policy directives, or plain inertia can cause enormous problems later on. But it is not always clear what disease an epidemic represents when it first appears, and this inhibits medical and public health authority responses. Sydney has experienced several epidemic situations where the authorities initially had no idea what they were dealing with, or how best to respond.
Smallpox in 1789
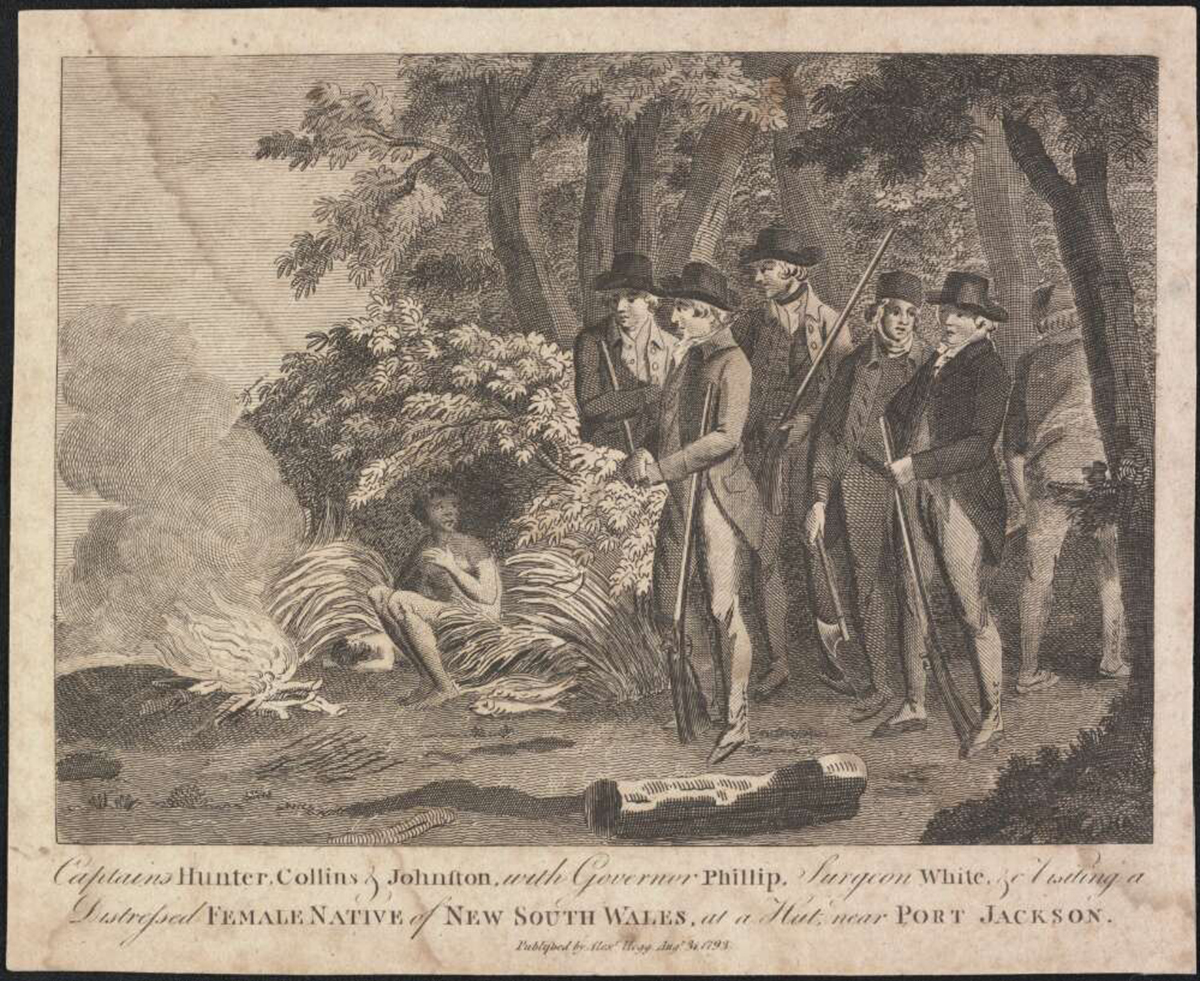
[media]During 1789 a major epidemic raged in Sydney. Even today its cause and point of origin are unclear, but historians suggest that it was either smallpox or chickenpox, probably smallpox. It was almost entirely confined to the Aboriginal community, and drew only confused and sluggish responses from white medical officers in the settlement.
This outbreak was short-lived but it exhibited a number of features that were repeated in later epidemics. Both its nature and origins were unknown, and the authorities were unsure how to respond. Its initial appearance amongst a group outside the mainstream of society meant there was little urgent pressure to react immediately. As it was of unknown origin, the search for its causes soon spilled over into a search for a scapegoat.
Rumours and theories fed on each other. Was it a disease indigenous to the country? Was it introduced by the white settlers in the First Fleet? Had it been brought by earlier explorers, from Dampier to Cook? Had it come from Norfolk Island? Had it been introduced by French seamen accompanying La Perouse in early 1788?
Modern evidence suggests that the smallpox epidemic was caused by the misuse of a bottle or bottles of 'variolus' matter which had been brought out from England for inoculation purposes. This material, accidentally or deliberately, infected some Aboriginal people and unleashed the epidemic.
Yet right from the very beginning a theory kept reappearing; that the disease had been introduced by the French. This idea was first discussed, and later rejected, in 1789, for good reason: the French ships were only at Botany Bay from January to March 1788, over a year before the epidemic broke out. There had been no evidence of smallpox on the French ships, and there was no evidence of it amongst the natives of Botany Bay in the intervening period. There was clearly no intermediary, yet the theory kept reappearing. In 1804, for example, the colony's principal surgeon noted that it
was generally accredited by the medical gentlemen of the colony ... that the smallpox had been introduced among the natives by the crews of the French ships then lying in Botany Bay. [2]
At this time France and Britain were enemies. The Napoleonic Wars were raging, so there was little incentive to be scrupulous about facts. The story was picked up by WC Wentworth in the 1820s, and he published it in one of his influential histories of the colony. He noted,
The smallpox … at the epoch of the foundation of the colony by Governor Phillip … committed the most dreadful ravages amongst the aboriginal natives. This exterminating scourge was probably introduced by the crews of the vessels of Monsieur de la Perouse, who remained for a short time in Botany Bay … and during his stay there, established an intercourse with the natives; although Captain Cook could not, with his utmost endeavours, effect this object. As they had, therefore, no communication with the seamen of Cook's vessel … it seems that they could only have caught this dreadful pox from the crews of the vessels belong to this celebrated French Navigator. [3]
[media]This interpretation passed into Australian history, although recent research has suggested a different story. Anti-French feeling was not prominent in Sydney in the early nineteenth century as there were very few French in Sydney during this period. But scapegoating 'the foreigner' did occur later on. In several of the other major epidemics, members of the Chinese minority were blamed.
Measles in 1866–67
Sydney has seen recurring epidemics of measles mainly among children. There were serious outbreaks of the disease in 1866–67, 1875, 1893, 1898, and 1920. The 1866–67 epidemic was one of the worst, because of the proportion of the population affected. There were some 8,600 cases in the colony of New South Wales, with possibly 80 per cent of children in Sydney under the age of five affected. There were some deaths, but most people recovered.
Scarlet fever in 1875–76
In terms of morbidity rates, the next major epidemic to engulf Sydney was the scarlet fever epidemic of 1875–76. As with measles, its victims were mainly children, and it led to more than 8,000 deaths in the Australasian colonies, with approximately 1,500 deaths in New South Wales, including almost 600 in Sydney. It is estimated that the death rate in Sydney was 32 per 1000, and in Waterloo and Alexandria, this figure was made worse still by an infant mortality rate which contemporary sources reported as 46 per cent of all births. [4]
But because it was a known disease, it did not lead to a major panic. The Sydney City and Suburban Sewage and Health Board, which had been appointed by the Colonial Secretary to investigate and report on a range of health issues affecting Sydney, outlined to the Legislative Assembly a range of responses that would minimise the impact of the epidemic. Restrictions on children attending school were introduced, policies of isolation and quarantine were put in place, and doctors visited the ill at their homes. As a result, the crisis passed without a great deal of public hysteria.
The Board had also collected a monumental quantity of evidence on the various health matters it investigated, and this provided a valuable database for dealing with future outbreaks of infectious diseases. Despite this, within a few years a new epidemic occurred, with disastrous results for some of Sydney's population.
Smallpox in 1881–82
The first case of smallpox reported in 1881 was of a Chinese child, the son of On Chong, one of Sydney's leading merchants. As the epidemic spread over the next few months, anti-Chinese feeling was fanned by the newspapers. The press in turn were deluged by letters calling for the expulsion of the Chinese and an end to their migration. Others suggested they should be vaccinated and forcibly incarcerated.
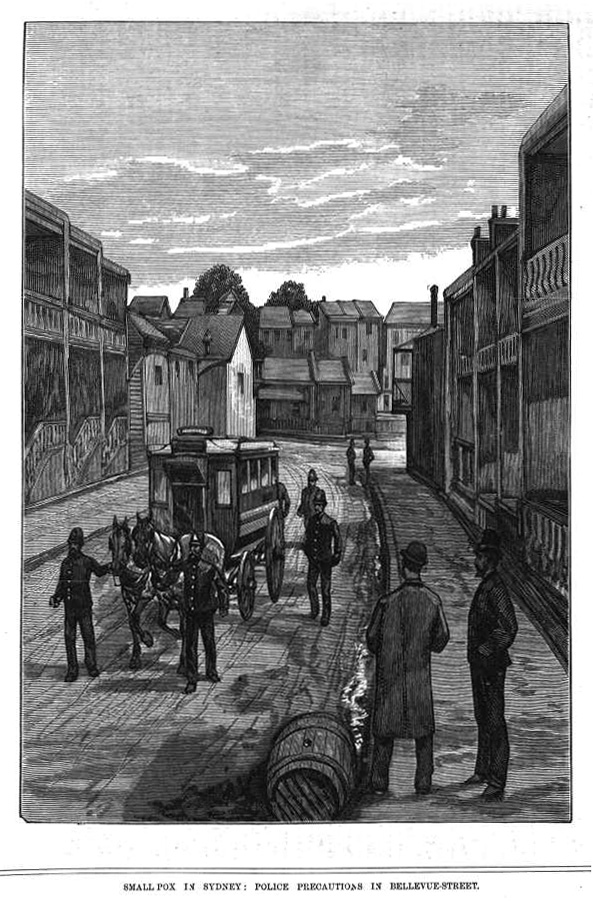
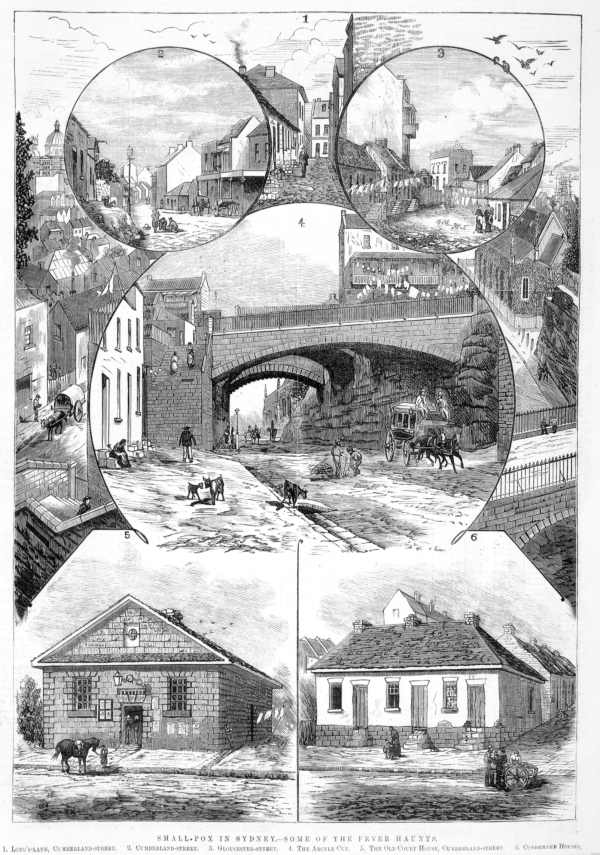
[media]The disease, combined with the hysteria and panic whipped up by the newspaper reports caused the wider community to turn quickly against the Chinese. The colonial government legislated to restrict all population movements between China and New South Wales and there was increasing public violence against individual Chinese. The colonial health authorities forcibly vaccinated the occupants of On Chong's house, and removed them to the Quarantine Station at North Head. The house of another Chinese person found to be infected, that of Won Ping in Waterloo, was burned down after he had been removed by health authorities. Health workers had refused to assist the ill man, and he was removed by the police 'using missiles and long poles.' [5]
Anti-Chinese feeling grew even stronger in the next few months. Rumours circulated that the Chinese were deliberately hiding their ill to avoid having them taken away. Chinese businesses were boycotted and many Chinese were refused entry onto trams. Some were forcibly ejected from shops and public places. Others were spat at and publicly humiliated in the streets. There were even moves by various residents and merchants to have the government remove all Chinese people from their local areas.
[media]While the most overt symptoms of anti-Chinese feeling died down after the epidemic was over, the prejudice clearly remained. During the plague of 1900, the Chinese were once again targeted for persecution. Many Chinese businesses closed as a result of boycotts. There is no reason to presume any direct connection between the Chinese and the smallpox epidemic of 1881–82 or the plague of 1900. But popular prejudice was fanned by fear and the need to scapegoat, and the Chinese community suffered as a result.
Asiatic flu in 1890
When the next pandemic reached Australia in 1890, it brought with it high levels of infection and morbidity. In Sydney, there were about 130,000 cases and 234 deaths. The disease was a familiar one, and it spread across all ethnicities in the city, which led to it being dealt with in a more rational manner.
It also brought with it new lessons. The existing isolation and quarantine procedures were found to be inappropriate for such a contagious disease, and so new policies were implemented. A major public education campaign was undertaken, using cartoons in the main city newspapers and magazines. Sydneysiders were urged to avoid crowds and home quarantine was introduced. Sales of cough, cold and flu remedies boomed, and the pandemic eventually petered out. One of its long-term effects may have been to encourage Sydneysiders to think more carefully about measures to protect their health.
Smallpox from 1913 to 1917
War, and a smallpox epidemic in Sydney from 1913 to 1917, brought new chaos to the city. The strain was a mild one, though very contagious – there were 2,019 cases in Sydney, but only four deaths in New South Wales. Because of the smallpox outbreak, the Commonwealth government imposed harsh travel restrictions on the city. An area 15 miles from the GPO was declared a quarantine area, with a fine of £50 for non-observance.
But the epidemic and the government response also had one beneficial effect. It brought about a debate on the virtues and advantages of vaccination, and whether it should be voluntary or compulsory. This led to a rush of people being vaccinated. Sydneysiders were forced to take personal steps to safeguard their own health. Smallpox has not been a problem in Sydney since.
Spanish influenza in 1918–19
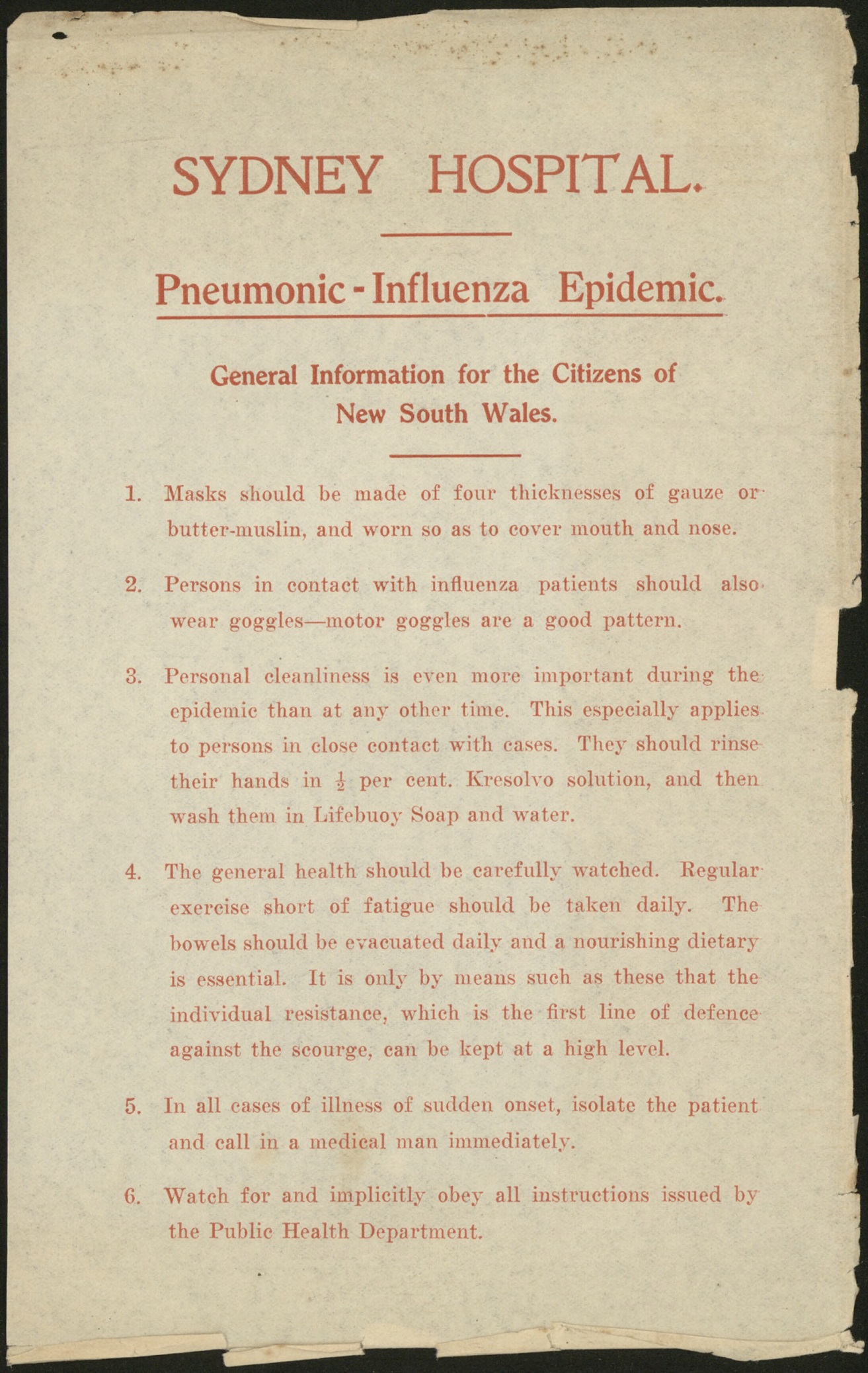
[media]The end of World War I brought peace, but also the worldwide onset of a particularly virulent form of influenza. This was not an epidemic confined to Sydney. Globally, it killed more people than the Great War. One fifth of the world's population was infected and some 50 million people died. Today many questions about its origins, its unusual epidemiological features, and the basis of its high fatality rates remain unanswered.
The name Spanish Flu came from the early outbreak and heavy mortality in Spain, where it allegedly killed eight million people, but the disease was soon seen in outbreaks around the world. [media]In the City of Sydney in 1919, 42 per cent of all deaths were from the flu, and there was ongoing and increasing pressure on health care facilities, with public hospitals unable to cope with the magnitude of the epidemic. Health authorities responded with sensible measures. Major public events were cancelled, public places were to be avoided, and the wearing of masks in public was made mandatory. Schools, cinemas and dance halls closed. But a lack of agreement between the relevant state and Commonwealth authorities meant that Sydneysiders often had to face conflicting policies, while media hysteria did little to help encourage public confidence.
HIV/AIDS from 1983
All the worst aspects of responses to epidemics came again in Sydney in the early 1980s, with the appearance of HIV/AIDS.
While AIDS is a disease which attacks people irrespective of sexual preference, it was first diagnosed in Western society among gay men. It thus became known as 'the gay plague', with consequent effects upon both gay communities and individual homosexuals. Later, when cases in other groups were found and its origins were traced beyond the homosexual subculture, many people still referred to it as 'the gay plague'.
When news of the first cases broke in the world press, attention was focused on the gay communities in America. When this was reported in the Australian press, immediate attention was drawn to Sydney's gay subculture, the largest collection of gay men in Australia, and where the first Australian cases were diagnosed. The unknown nature of the disease, its apparent deadliness, and its association with a minority only recently 'discovered' and only gradually being accepted by the population at large, meant that responses were unlikely to be favourable.
Sympathetic they certainly were not. As the journalist Evan Whitton noted in August 1985 in an article tellingly entitled 'AIDS: The Media, Paranoia and the Wrath of God', the
high level of AIDS induced paranoia may be ascribed to a number of factors: ignorance, fear – not of what has happened but of what might happen – medical scaremongering, media reportage and political overreaction. [6]
There was also deliberate fanning of prejudices by homophobes, with Christian fundamentalists at the forefront, who suggested that AIDS was God's response to the perverted ways of homosexuals. Yet as one writer noted,
since the incidence of AIDS amongst the other major homosexual group in our society, lesbians, is extremely low, then one can only presume that the Christian god must have been swayed by recent feminist arguments and so showed favoured treatment to women, or perhaps found himself confronting an Earth Mother or some other powerful deity protecting these women. [7]
Another result of these epidemics has been that society has come to know far more about the lifestyles and problems of various minority groups within it. The epidemics of the 1880s and 1900 brought to light much information on the Chinese, which in the long run helped dispel some misconceptions which fostered prejudice and persecution. The 1870s scarlet fever epidemic and the plague of 1900 uncovered much about the living conditions of the city's poor. And the AIDS epidemic has brought the existence of the sizeable and long-hidden gay community to the notice of mainstream Australian society.
Another ironic result of the impact of the AIDS years has been an improvement in the level of sexual knowledge, in the wider community and particularly in schools. Sex education programmes have been significant here. Time magazine noted that 'condoms and sex [are] discussed openly on television like recipes on a cooking show', and has made the following perceptive summation:
What liberals in large parts of the Western world have advocated in vain for decades, the fear of AIDS has achieved in a couple of years. [8]
Yet rational discussion of the causes of various epidemics, and how to deal with them, had its opponents. Bigotry and prejudice have often interfered with public health policies and responses. Unfortunately, religious leaders have often been in the forefront of those sending the wrong signals.
Religious responses
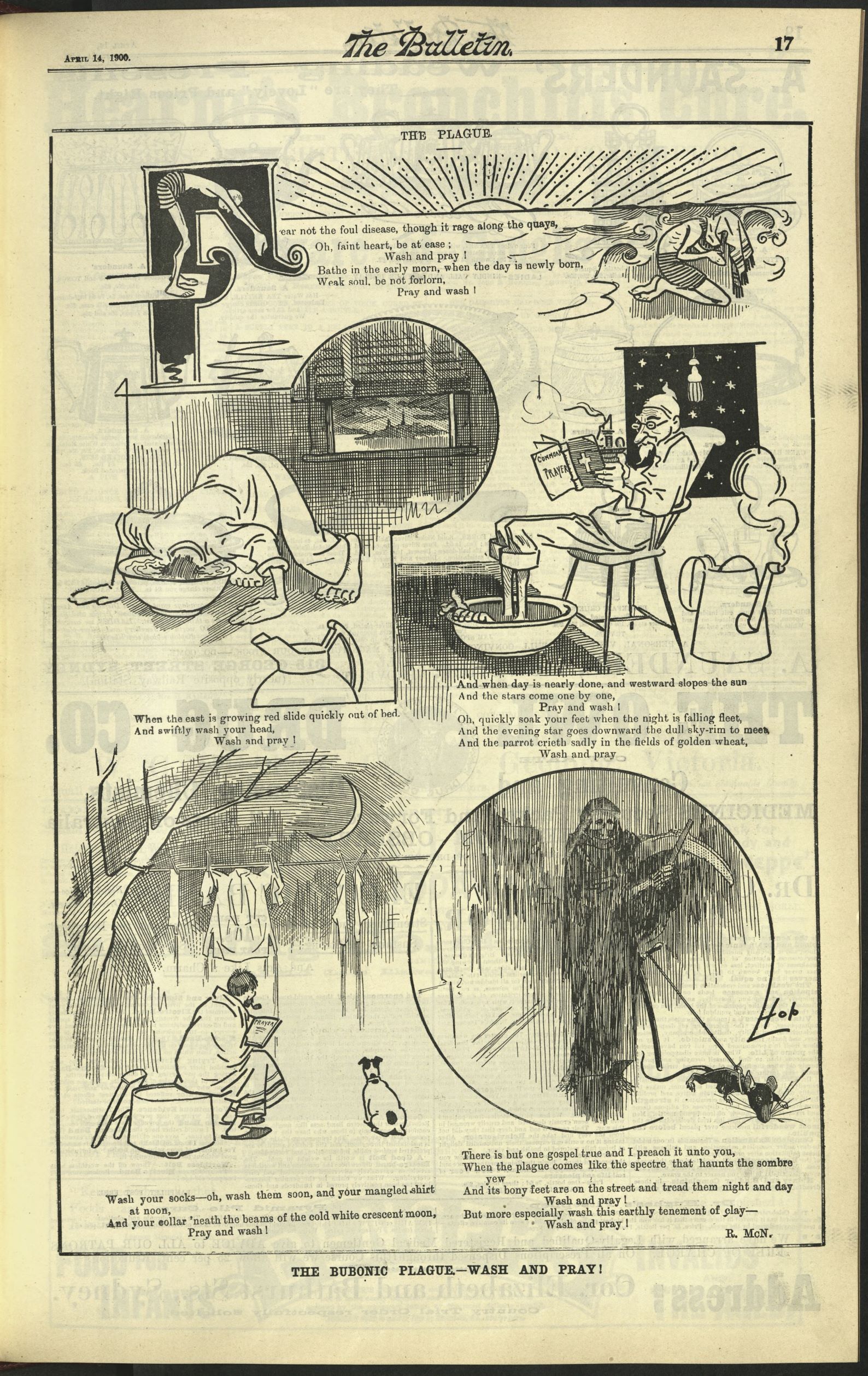
[media]For medical authorities attempting to determine causes, and thus choose responses, the situation was often exacerbated by interpretations put forward by the churches. There were often suggestions that an epidemic was divine wrath brought forth to punish the sinfulness of mankind. In the 1890 influenza epidemic and the plague in 1900, as with the influenza outbreak of 1919, religious leaders declaimed that plagues and pestilences, like those sent upon the land of Egypt, occurred because god was displeased.
Thus in November 1890, at the height of the Asiatic flu epidemic, the Bishop of Sydney drew up a special prayer to be read in all Anglican churches, requesting God to withdraw the pestilence from his people. Similarly, the 1900 plague was seen by the Christian churches as being yet another expression of divine wrath. There were constant prayers to intervene. At the height of the epidemic all the churches set aside a special day for public repentance, humiliation and prayer. On that day the churches were packed to overflowing.
Public health responses
Accurate, factual and readily available information was critical in the early stages of an epidemic. It allayed fears, and countered the misinformation put out by the ignorant and prejudiced. Accurate information was also important in underpinning the responses of government and health authorities.
In the 1789 epidemic, there was no consensus among the colony's medical men as to what the disease was, or how it had been introduced. As such, there was no official policy on how to deal with it. But since there was no effective treatment, this would not have mattered.
In the 1881–82 smallpox epidemic, one of the first measures the government took was to declare China and all its ports 'infected places', apparently because Chinese people had been among the earliest reported cases. This move allowed the government to quarantine all ships arriving from China so that it was seen to be doing something. But as the Sydney Morning Herald perceptively noted, 'considerable doubt exists whether the disease (was) brought here by the Chinese … we have far more to fear from our own countrymen than from the Chinese.' The Herald wanted to know what other measures the government was undertaking and it lead the considerable and mounting criticism of the government's handling of the public health problem. There was a lack of coordination between the various departments dealing with the epidemic, and a perception that popular prejudices and misinformation were being allowed to determine how people were dealt with. Hundreds of people were forcibly quarantined, simply because they had been reported by neighbours for 'suspicious' behaviour. Tragically, many uninfected people caught the disease when they were forcibly quarantined. Others were detained aboard ships on arrival in Sydney. Families quarantined in their houses were left to fend for themselves and the various authorities failed to coordinate who was to bring them fuel and food. [media]A man who wore bandages to hide a disfigured face was detained by police in public and sent to North Head quarantine station, where he was kept for five weeks. He was lucky as he survived. But his business was in ruins when he was released, and he received no compensation from the government.
In this epidemic it is clear that many individual legal rights were ignored. The economic cost of government action was never acknowledged and the government refused to take responsibility for the actions done in its name. After the epidemic had died down, the Sydney Morning Herald noted in a scathing editorial that 'the Government must be held to have blundered a good deal at first', although it did concede that politicians had 'learned wisdom as they went on.' [9]
Yet paradoxically, the responses to these epidemics brought about unforeseen long–term beneficial results in a variety of ways. Pressure built up to reform existing inefficient practices, and to search for more accurate factual information about diseases, their origins and means of transmission. New ways of looking at public health problems emerged, placing them in the context of social problems such as overcrowding, poverty and poor sanitation. All these results are evident in varying degrees in the different epidemics which have swept Sydney.
[media]Thus the scarlet fever epidemic of the 1870s produced widespread concern over the inadequacy of public health and sanitation. Because many of its victims were middle class, the government was forced to respond to articulate and highly critical attacks on its actions. As a result, a series of government sponsored investigations were established to look into this disease, which brought to light useful information on the origins, prevalence and means of transmission of diseases in general. It also resulted in the first tentative steps towards establishing official policy in New South Wales on the control and management of epidemics.
The 1881–82 smallpox epidemic helped lay the foundations of public health administration in New South Wales. As Curson notes,
A Board of Health, an Infectious Diseases Act, an infectious diseases hospital (the Coast Hospital), the Medical School at Sydney University and a set of practical regulations and guidelines governing quarantine, isolation and the general management of epidemics, all owe their origin to the (1881-2) epidemic. [10]
Curson has also suggested that the plague of 1900 in fact constituted,
a blessing in disguise for it served to draw attention to the insanitary and depressed living conditions of many city dwellers and to the fact that Sydney was an ill-regulated and ill-governed city. It also led to ... increasing pressure for sanitary, health and local government reform. [11]
[media]Putting out simple factual information was of major importance in the influenza epidemic of 1919. It gave people plain guidelines about how to protect themselves from the contagion, by avoiding public places and crowds, and using face masks to avoid inhaling airborne [media]germs.
Thus the various epidemics, despite their costs and harrowing personal impacts, brought reforms that improved procedures and practices in the various departments constituting the health authorities. They also focused attention on the need for better information, and ways to make it available. [media]By the early twentieth century, health authorities knew far more about overcrowding and the role of unsanitary living than they had 10 or 20 years earlier. This information allowed them to devise new ways of dealing with, and responding to, epidemics.
The media in epidemics
The first epidemic in which the newspapers played a major role was the smallpox epidemic of 1881–82. Advertisements and stories about 'The Great Plague' and 'The Black Death' fanned the rising panic. Many reports and pamphlets were produced by Sydney's medical men, usually offering contradictory diagnoses and treatment of particular cases. All of these helped inflame popular opinion, and even though the morbidity and mortality produced by this epidemic were small, its social impact was tremendous.
Similarly, the newspapers played a major role during the plague outbreak of 1900, determining how social responses to the disease developed. They ran daily reports on the epidemic, ranging from factual day-to-day reports of the progress of the disease (including lists of victims and their addresses), the fate of earlier victims and the location of quarantine premises. They also published vivid accounts of earlier plagues and the fearful mortality that they provoked, together with articles by medical 'specialists' often giving contradictory expert opinions.
[media]The newspapers also played their part in the scapegoating process. In 1900 Sydney newspapers were full of charges against the Chinese community, claiming that they were responsible for introducing the disease and for hiding away those of their number who caught the plague. For the mass of the population who relied on the press for knowledge about the disease, this fostered confusion and prejudice against those the newspapers blamed for the outbreak of the disease.
In the twentieth century, Sydney newspapers reacted similarly to AIDS. The disease was first reported in December 1981, and until May 1983 most stories were speculation about the nature and course of the disease. It was first diagnosed here in March 1983, although parts of the gay press had already been reporting on it. For example, one article in 1982 noted the unusually large number of cases of Kaposi's sarcoma – a form of cancer usually found in elderly Mediterranean men – appearing in European and American gay communities.
Late in May 1983 the Sydney Daily Mirror ran the headline 'AIDS: The Killer Disease that's expected to sweep Australia'. This appeared to start the homophobic panic. Fred Nile, a Christian minister and parliamentarian, responded by demanding that homosexuals be prevented from entering or leaving the country, and that all gay venues be closed.
Misinformation surfaced, even in places from which one might have expected better. For example, The Medical Journal of Australia, in its June 1983 issue, showed on its cover a skull and an X-ray, and carried the headline 'The Black Plague of the Eighties...perhaps we've reached a situation like this to show us what we've known all along – depravity kills.' In the face of the resulting outcry, the editors claimed that they had tried a 'satirical approach', but if this was satire, it backfired. [media]People had taken the message literally, and the MJA was forced to issue an apology in a later issue.
Yet the same media can also argue for calm, and disseminate factual information. The Sydney Morning Herald editorial suggesting that there was no proof that the smallpox epidemic of 1881–82 was 'caused' by the Chinese is a case in point. And in 1900 various responsible newspapers took a reasoned stance. In March of that year the Bulletin editorialised that,
So far the Plague ... is a very small affair. It isn't a patch on the daily, hourly typhoid as a means of slaughtering the public, and so far it has proved about as safe as football, and much safer than it was a few weeks ago to have doubts concerning the absolute justice of the war in South Africa. [12]
It attempted to put the plague in the context of the hazards of everyday life.
The need for readily available, clear and factual information is obvious. Without this, doubt, confusion and prejudice can take over and scapegoating will occur with far greater long-term costs. It is also clear that human behaviour can be modified by sensitive and appropriate education, such as sex education in schools which has helped to limit the spread of AIDS.
The role of certain institutions, like churches and the media, also needs careful attention. In a democratic society, the conflicting aims of protecting public health, ensuring the safety of society, protecting individual rights, and maintaining the freedom of the press from interference, have to be balanced. Epidemics will continue to occur, and may be more likely now that globalisation brings with it fast air travel and large population movements. A new epidemic, regardless of where it starts, will now travel round the world and reach Sydney in days rather than months. Sydney's history shows that if care is not taken, hysteria, panic and prejudice can take over very quickly.
References
P Curson, Times of Crisis: Epidemics in Sydney 1788–1900, Sydney University Press, Sydney, 1986
Anthea Hyslop, 'Epidemics', in G Davison, J Hirst and S Macintyre (eds) , The Oxford Companion to Australian History, Oxford University Press, Melbourne, 1998
WH McNeill, Plagues and Peoples, Knopf, London, 1985
Notes
[1] P Curson, Times of Crisis: Epidemics in Sydney 1788-1900, Sydney University Press, Sydney, 1986, p xi
[2] Sydney Gazette, 14 October 1804
[3] C Wentworth, A Statistical Account of the British Settlements of Australasia, Geo B Whittaker, London, 1824, pp 310–11
[4] Illustrated Sydney News, 19 July and 13 September 1890, quoted in M Cannon, Life in the Cities, Currey O'Neil Ross, South Yarra, 1983, p 128
[5] P Curson, Times of Crisis: Epidemics in Sydney 1788–1900, Sydney University Press, Sydney, 1986, p 105
[6] Evan Whitton, 'AIDS! The Media, Paranoia, and the Wrath of God', Sydney Morning Herald, 17 August 1985, p 41
[7] G Wotherspoon, City of the Plain: history of a gay sub-culture, Hale and Iremonger, Sydney, 1991, pp 223–24
[8] 'Global War on AIDS', Time, 25 May 1987, p 42
[9] Sydney Morning Herald, 2 February 1882, p 4
[10] P Curson, Times of Crisis: Epidemics in Sydney 1788–1900, Sydney University Press, Sydney, 1986, p 91
[11] P Curson, Times of Crisis: Epidemics in Sydney 1788–1900, Sydney University Press, Sydney, 1986, p 164
[12] Bulletin, 31 March 1900, p 6
.